Occupational therapy (OT) plays a pivotal role in the rehabilitation journey of individuals who have sustained a spinal cord injury (SCI). An SCI can have life-altering consequences, impacting a person's ability to carry out personal activities of daily living, such as bathing and dressing, and instrumental activities of daily living, such as cooking and cleaning. Occupational therapy helps empower individuals to regain their independence, achieve optimal functionality, and improve their overall quality of life.

In this article, we will focus on how occupational therapy contributes to the multidisciplinary approach to SCI rehabilitation, delving into the techniques, strategies, and interventions that optimize recovery and promote reintegration into daily life.
Understanding Spinal Cord Injuries
An SCI refers to damage sustained by the spinal cord, a critical part of the central nervous system that facilitates communication between the brain and the rest of the body. The spinal cord is responsible for transmitting sensory, motor, and autonomic signals, which control various functions such as movement, sensation, and the regulation of internal organs. Injuries to the spinal cord from various causes, including trauma (e.g., motor vehicle accidents, falls, sports injuries), diseases (e.g., tumours, infections), or congenital disorders, can lead to temporary or permanent impairments in sensation, movement, strength, and physiological functions at or below the site of injury (Spinal Cord Injury, n.d.).
Symptoms
Symptoms of spinal cord injuries (SCI) vary depending on the location and severity of the injury. Injuries higher up on the spinal cord can lead to paralysis of most of the body, affecting all limbs (tetraplegia or quadriplegia). In contrast, an injury lower down on the spinal cord might cause paralysis of the legs and lower body (paraplegia).
Another factor that affects the severity depends on whether the injury is incomplete or complete. Incomplete injuries allow some nerve messages to be transmitted, preserving partial sensory function and muscle control. In contrast, complete injuries result in a total loss of nerve communication and are more severe. Some common symptoms of SCI include:
Loss of movement: Paralysis or weakness in muscles below the level of injury may occur, affecting the ability to move limbs or control muscle tone.
Altered sensation: Individuals may experience a decreased or complete loss of sensation, including the ability to feel touch, temperature, or pain below the level of injury.
Spasticity: Involuntary muscle contractions or increased muscle tone can develop in affected limbs.
Pain: Neuropathic or musculoskeletal pain may arise due to nerve damage or muscle and joint function changes.

Bowel and bladder dysfunction: Control over bowel and bladder function may be impaired, leading to incontinence or the need for assistance in managing these functions.
Respiratory issues: Injuries to the cervical spinal cord may affect the muscles responsible for breathing, resulting in difficulties with respiration or the need for mechanical ventilation.
Circulatory problems: Blood pressure fluctuations, blood clots, and orthostatic hypotension may develop due to altered autonomic nervous system function.
(Acute Spinal Cord Injury, 2021)
How SCIs Impact Daily Living
Spinal cord injuries can have a profound impact on daily living, as they often result in a range of physical, emotional, and social challenges:
People with spinal cord injuries (SCI) may encounter various physical challenges that make performing routine activities, such as self-care, mobility, and preparing meals, difficult. These challenges may arise due to muscle weakness or spasticity, pain, pressure sores, and problems with bowel and bladder function.
Apart from physical difficulties, individuals with SCI may also face emotional challenges such as frustration, depression, anxiety, and grief. Losing the ability to perform daily tasks and being dependent on others can be emotionally draining. As a result, seeking psychological support to manage these difficulties is essential for a better quality of life.
In addition, SCI can have social implications, affecting relationships, work, and leisure activities. Adapting to changes in physical abilities may require re-evaluating roles and responsibilities within the family, workplace, and community. Social and recreational activities may be limited due to accessibility barriers or the need for assistance, leading to feelings of isolation and reduced quality of life.
(Occupational Therapy and Spinal Cord Injury, n.d.)
“Once you choose hope, anything’s possible.” – Christopher Reeve, Actor and Founder of the Christopher and Dana Reeve Foundation

Photograph: Christopher Reeve is best known for playing the title character in the film Superman. On May 27, 1995, Reeve broke his neck when he was thrown from a horse during an equestrian competition in Culpeper, Virginia.
Occupational Therapy Assessment Process for Spinal Cord Injury
Occupational therapists (OTs) are crucial in evaluating and managing patients with spinal cord injuries (SCI). They assess an individual's functional abilities by focusing on various aspects such as upper limb strength, fine motor skills, sensation, coordination, and cognitive skills. Additionally, they examine the patient's ability to perform daily living activities, including self-care tasks, mobility, and work or leisure-related activities.
Standardized assessment tools like the Spinal Cord Independence Measure (SCIM) or the Canadian Occupational Performance Measure (COPM) are also used by occupational therapists to evaluate a patient's functional status and identify areas that require intervention. Moreover, OTs assess environmental factors, such as home or workplace accessibility, to determine the need for modifications or adaptive equipment to enhance a patient's independence and participation in daily activities.
Spinal Cord Independence Measure
The Spinal Cord Independence Measure (SCIM) is a standardized assessment tool specially designed to evaluate the functional independence of individuals with spinal cord injuries. It considers the unique challenges and limitations associated with SCI to measure their ability to perform daily activities.
The SCIM is divided into three main categories: self-care, respiration and sphincter management, and mobility. These categories are divided into 19 subcategories, covering various aspects of daily living, such as dressing, bathing, eating, bladder and bowel management, mobility in different environments, and transferring between positions (Spinal Cord Independence Measure, n.d.).
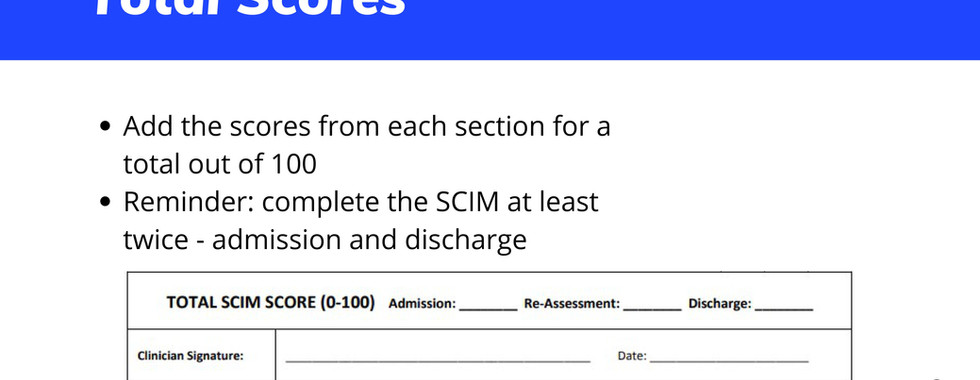
Each subcategory is scored on a scale based on the level of assistance required, with higher scores indicating greater independence. The scores from each subcategory are then totalled to provide an overall score ranging from 0 (complete dependence) to 100 (complete independence).
Occupational therapists and other rehabilitation professionals use the SCIM to identify areas of need, set appropriate intervention goals, and track progress in individuals with spinal cord injuries. Using SCIM facilitates optimal recovery and enhances participation in daily activities for individuals with SCI.
Check out the following slider presentation for a more thorough look at the SCIM.
Download the interactive PDF here (it only works with Adobe Acrobat Reader):
Tailored Therapy Plans
A tailored therapy plan for someone with an SCI is developed based on the individual's unique needs, injury level, and functional capabilities. The plan typically involves a multidisciplinary approach, with input from various healthcare professionals such as occupational therapists, physical therapists, psychologists, and other specialists as needed.
Components of a tailored therapy plan for an SCI patient may include:
Mobility and transfer training: Focuses on improving the patient's ability to move, transfer between different positions, and use assistive devices like wheelchairs, walkers, or braces.
Upper limb and fine motor skill rehabilitation: Enhances strength, dexterity, and coordination in the hands and arms, enabling the patient to perform daily tasks more effectively.
Self-care and activities of daily living (ADL) training: Teaches and practices strategies for managing personal care tasks, such as bathing, dressing, and eating independently or with minimal assistance.
Bladder and bowel management: Develops routines and techniques to manage bladder and bowel functions and maintain hygiene effectively.
Respiratory therapy: Strengthens respiratory muscles and teaches breathing techniques to improve lung function and reduce the risk of respiratory complications.
Adaptive equipment: Assesses and recommends appropriate adaptive equipment and assistive technologies to enhance independence and facilitate daily tasks.
Home and workplace modifications: Evaluates the patient's environment and suggest necessary modifications to ensure safety, accessibility, and functional independence.
Pain management: Implements strategies and interventions to manage and alleviate pain, such as medication, physical therapy, and relaxation techniques.
Psychological support: Addresses the emotional and mental health aspects of living with an SCI through individual counselling, support groups, or family therapy.
Vocational and recreational therapy: Assists the patient in exploring suitable work or leisure activities that accommodate their abilities and interests, promoting social integration and a sense of purpose.
(The Role of Occupational Therapy in Acute Spinal Cord Injury, n.d.)
Regular monitoring and adjustments to the therapy plan are essential to ensure that the individual continues progressing towards their rehabilitation goals and achieves the highest possible level of functional independence and quality of life.
Example - A closer look at upper limb and fine motor skill rehabilitation:
At the beginning of the upper limb rehabilitation program, the occupational therapist assesses the patient's current strength, range of motion, coordination, dexterity, and sensation to identify areas that need intervention and establish a baseline. Based on this assessment, the therapist creates a tailored exercise program to improve muscle strength, flexibility, and joint mobility in the affected limbs, which may include resistance training, passive stretching, and active range of motion exercises.
Example Therapy Instruction Worksheet:
Week 1-2: Upper Limb and Fine Motor Skill Exercises
A. Strengthening and Range of Motion Exercises:
Wrist Flexion and Extension:
With your forearm resting on a table and your hand hanging over the edge, gently bend your wrist up and down.
Repeat 10 times, perform 3 sets, twice a day.
Finger Flexion and Extension:
Place your hand flat on a table and slowly lift each finger, one by one.
Repeat 10 times, perform 3 sets, twice a day.
Elbow Flexion and Extension:
Sitting or standing, bend your elbow to bring your hand towards your shoulder, then straighten your arm.
Repeat 10 times, perform 3 sets, twice a day
B. Fine Motor Skill Exercises:
Coin Pickup:
Scatter several coins on a table and pick them up one by one, placing them in a container.
Perform for 5 minutes, twice a day.
Pinch Strength:
Pinch a clothespin or clip between your thumb and each fingertip.
Hold for 5 seconds, repeat 10 times for each finger, twice a day.
Stringing Beads:
Using a shoelace or string, thread beads or buttons with various sizes and shapes.
Perform for 5 minutes, twice a day.

Week 3-4: Upper Limb and Fine Motor Skill Exercises
A. Strengthening and Range of Motion Exercises:
Forearm Pronation and Supination:
With your elbow bent at 90 degrees and your forearm supported on a table, rotate your palm up and down.
Repeat 10 times, perform 3 sets, twice a day.
Shoulder Flexion and Extension:
While seated or standing, lift your arm straight in front of you, up to shoulder level, and then lower it back down.
Repeat 10 times, perform 3 sets, twice a day.
Shoulder Abduction and Adduction:
While seated or standing, lift your arm straight out to the side, up to shoulder level, and then lower it back down.
Repeat 10 times, perform 3 sets, twice a day.
B. Fine Motor Skill Exercises:
Chopsticks Exercise:
Pick up small objects, such as beads or beans, using chopsticks or tweezers, and transfer them to another container.
Perform for 5 minutes, twice a day.
Finger Opposition:
Touch the tip of your thumb to the tip of each finger in sequence, starting from the index finger to the little finger, and then reverse the sequence.
Repeat 10 times, perform 3 sets, twice a day.
Rubber Band Extension:
Loop a rubber band around the tips of your fingers and thumb. Spread your fingers apart against the resistance of the rubber band.
Hold for 5 seconds, repeat 10 times, perform 3 sets, twice a day.
As you may have noticed, the exercises in Weeks 3 and 4 of the rehabilitation program were progressively more challenging. This is because it's crucial to gradually increase the difficulty of exercises to meet the evolving needs and demands of the patient. This progressive approach promotes functional improvement and fosters motivation and engagement in the therapy process. By carefully adjusting exercise intensity and complexity, occupational therapists ensure that individuals with spinal cord injuries continue to make progress, ultimately enhancing their independence and overall quality of life.
The Vital Role of Occupational Therapy in SCI Rehabilitation
Occupational therapy plays a critical role in SCI rehabilitation. Occupational therapists collaborate with SCI patients and other healthcare professionals to develop personalized therapy plans that address their unique needs and goals. They focus on improving functional independence, enhancing the quality of life, and facilitating reintegration into daily life activities, work, and leisure pursuits. By employing a holistic approach that considers the physical, psychological, and social aspects of living with an SCI, occupational therapists help individuals adapt, regain autonomy, and lead fulfilling lives.

References (click or tap to expand)